Sleep Apnea Across the Lifespan in People with Down Syndrome
Takeaways from a GLOBAL Webinar

Article from the award-winning Down Syndrome World™ magazine.
Learn more about our magazine, webinars and GLOBAL Membership benefits
Sleep Apnea Experts
Earlier this year, GLOBAL organized a webinar on sleep apnea that attracted 420 registrants from 43 states and 13 countries. The webinar covered the latest understanding of the importance of sleep screening across the age spectrum in people with Down syndrome, consequences of untreated sleep apnea, medical treatment options, and surgical treatment options including hypoglossal nerve stimulation.
Dr. Ignacio Tapia and Dr. Rachel Whelan co-presented the webinar, and the hour and fifteen minutes flew by! Dr. Tapia is an attending physician in the Sleep Center/Pulmonary Division of the Children’s Hospital of Philadelphia (CHOP) and Associate Professor in Pediatrics at the Perelman School of Medicine at the University of Pennsylvania. Dr. Tapia’s research interests are specific to Obstructive Sleep Apnea Syndrome (OSAS) in children, clinical trials to treat OSAS in children, health disparities around sleep and OSAS in individuals with Down syndrome. OSAS is the day-time sleepiness and fatigue associated with OSA.
Dr. Whelan is an Assistant Professor of Otolaryngology at the University of Pittsburgh Medical Center (UPMC) and specializes in the treatment of sleep disorders in pediatric and adult patients. She has dual fellowship training in both pediatric otolaryngology and sleep medicine through UPMC and the University of Pennsylvania/CHOP. Dr. Whelan has a particular focus in surgical treatment options for sleep-disordered breathing including nasal, pharyngeal, and neurostimulation surgeries and enjoys caring for patients across the age spectrum.
What is Obstructive Sleep Apnea?
According to the Mayo Clinic, Obstructive Sleep Apnea (OSA) is the most common sleep-related disorder and occurs when the throat muscles relax and block the airway repetitively during sleep. Essentially, people with OSA stop breathing, sometimes for more than 10 seconds, and then start breathing again which negatively affects their sleep and overall health.
In the United States, it is estimated that 15% of adult males and 5% of adult females have OSA, and that it affects 1-5% of all children. Obesity is an independent high-risk factor whereby upwards of 20% of adults and 70% of children with obesity were also diagnosed with OSA.
Generally, it is a bed partner or parent who identifies OSA since snoring is a key symptom. To be clear, many people snore and do not have OSA but snoring, restless sleep, uncommon sleep positions such as sit sleeping, night waking, audible pauses in breathing, dry mouth, headaches, daytime sleepiness, and behavioral problems including mood swings, are all symptoms that should be mentioned to a health care provider, as these may raise concern for possible sleep apnea.
Increased Risk in People with Down Syndrome
Drs. Tapia and Whelan both emphasized that people with Down syndrome are at significantly increased risk through their lifespan for developing OSA, with somewhere between 45-55% of individuals with Down syndrome having Obstructive Sleep Apnea Syndrome (the fatigue, cognitive deficit and behavior issues associated with poor sleep due to OSA).
The increased risk can be attributed to a combination of multiple factors:
- Anatomy
- Midface hypoplasia (narrowing of the upper airway and back of the nose)
- Glossoptosis and macroglossia (the tongue is larger relative to the jaw) and thus more likely to fall back and block the airflow in the back of the throat
- Hypotonia (low muscle tone) which also increases collapse of the upper airway
- Large tonsils and adenoid tissue in the back of the throat and nose, respectively
- Co-occurring obesity
- Hypothyroidism
Because of this significantly increased risk, the American Academy of Pediatrics (AAP) in the US recommends “evaluation” at age 6 months and a Polysomnography (PSG), overnight sleep study, by age 4 years. Currently there are no medical guidelines specific to adults with Down syndrome (guidelines for the general population are the default) but the Global Down Syndrome Foundation is working on their second edition of the GLOBAL Medical Care Guidelines for Adults with Down Syndrome that will expand five medical areas including recommendations for OSA.
Challenges for OSA Patients with Down Syndrome
Short term, untreated OSA in all patients results in fatigue and mood swings. According to Johns Hopkins University, this can manifest in daytime car accidents, loss of productivity at work, waking up groggy, falling asleep in class, and behavioral issues that make it difficult to study or pay attention to schoolwork.
It makes sense that lack of a deep sleep and poor-quality sleep is not good for you. But for OSA, the long-term consequences can be dire, including neurobehavioral deficits, increased risk of high blood pressure , metabolic issues such as diabetes, and a possible link with early onset of Alzheimer’s disease.
During the GLOBAL Webinar on sleep apnea, Dr. Tapia highlighted three key challenges that people with Down syndrome face with both the diagnosis and the treatment: (1) there are very few sleep labs (2) The sleep study test is challenging and the majority of children with Down syndrome don’t get the study despite the AAP guidelines, and (3) patients with Down syndrome have had difficulty with adhering to continuous positive airway pressure (CPAP) and many families feel it is unrealistic to expect adherence.
Dr. Tapia also spoke about people with Down syndrome not being invited to participate in research over the last few decades and how that has led to so many unknowns about sleep apnea in the Down syndrome community. He also kindly acknowledged GLOBAL’s great lobbying work in DC that led to the establishment of a National Institutes of Health (NIH) Down syndrome research funding program called INCLUDE.
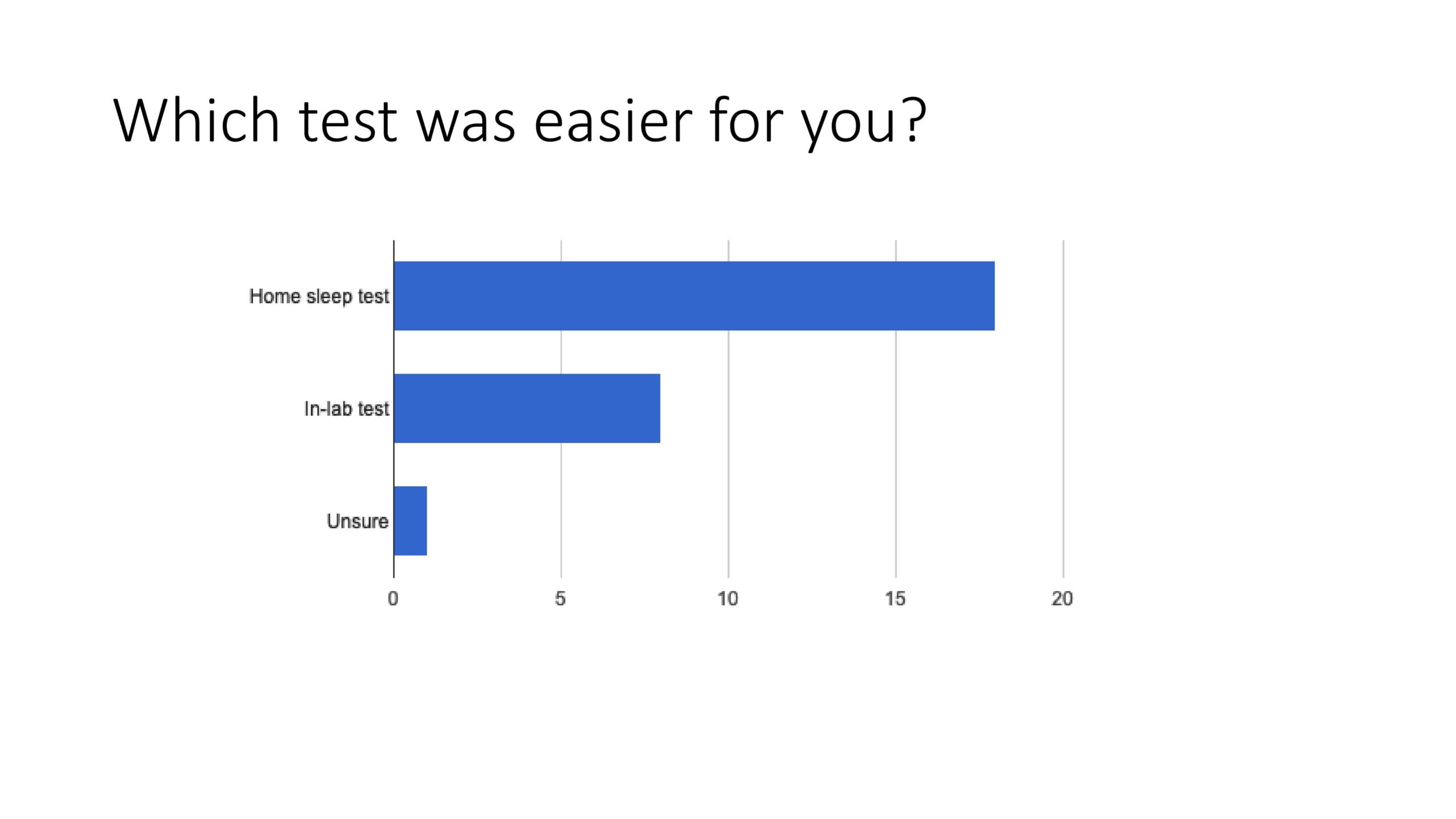
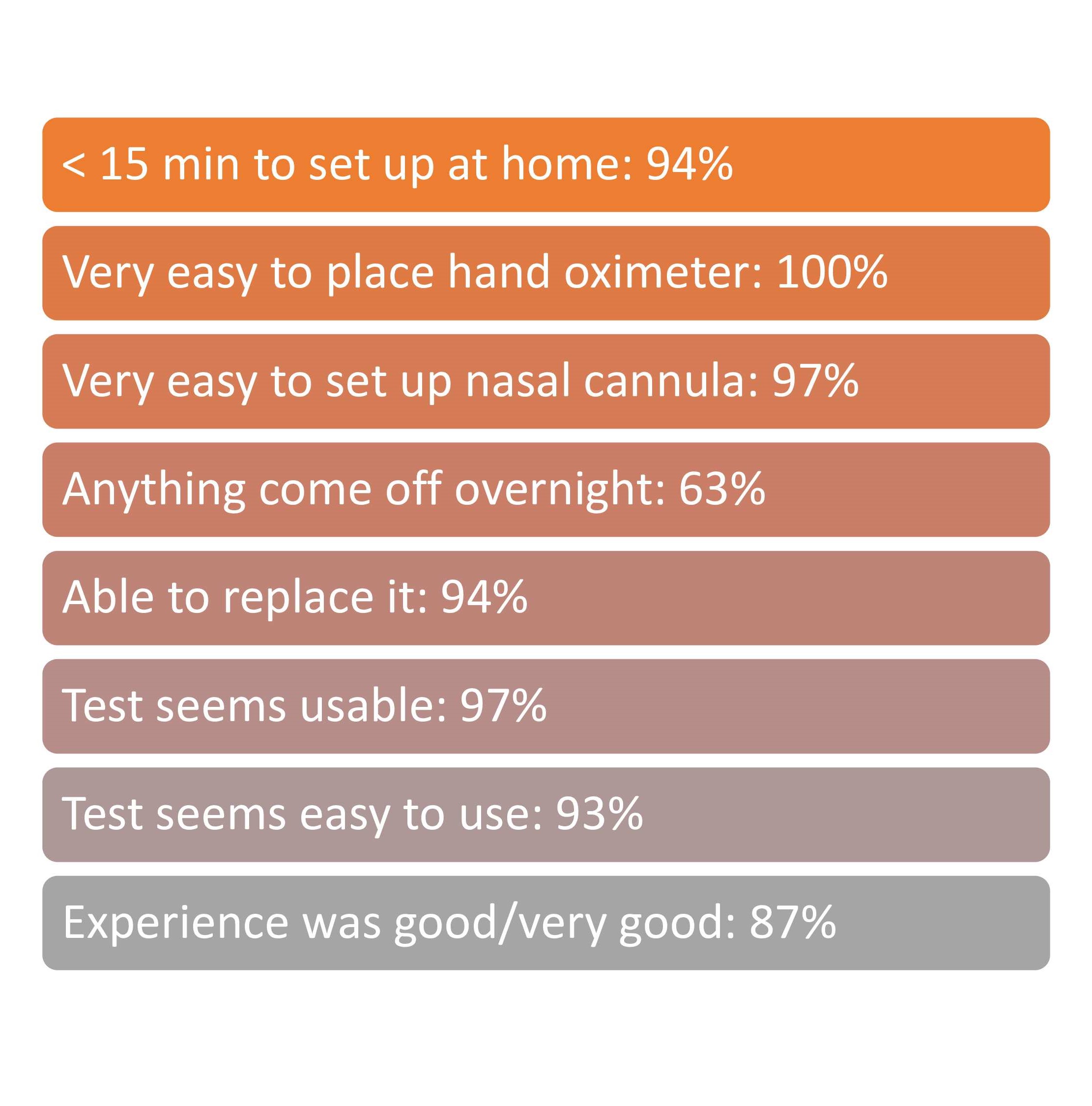
Dr. Tapia shared that he has received two INCLUDE grants, one of which is targeted at proving that home sleep study tests are not only possible but preferable in children with Down syndrome. This could solve two of the key problems associated with diagnosis of OSA. The study tested 35 patients with Down syndrome between 10 and 20 years of age, and compared at home study results versus lab study results measuring tolerability, family-report sleep perceptions/experience, feasibility, and diagnostic accuracy for moderate-severe OSA.
The majority of participants felt that the home study test was easier and the overall ease of the setup of the home test was an aggregate score of 87%.
The results were recently published in the Journal of Clinical Sleep Medicine:
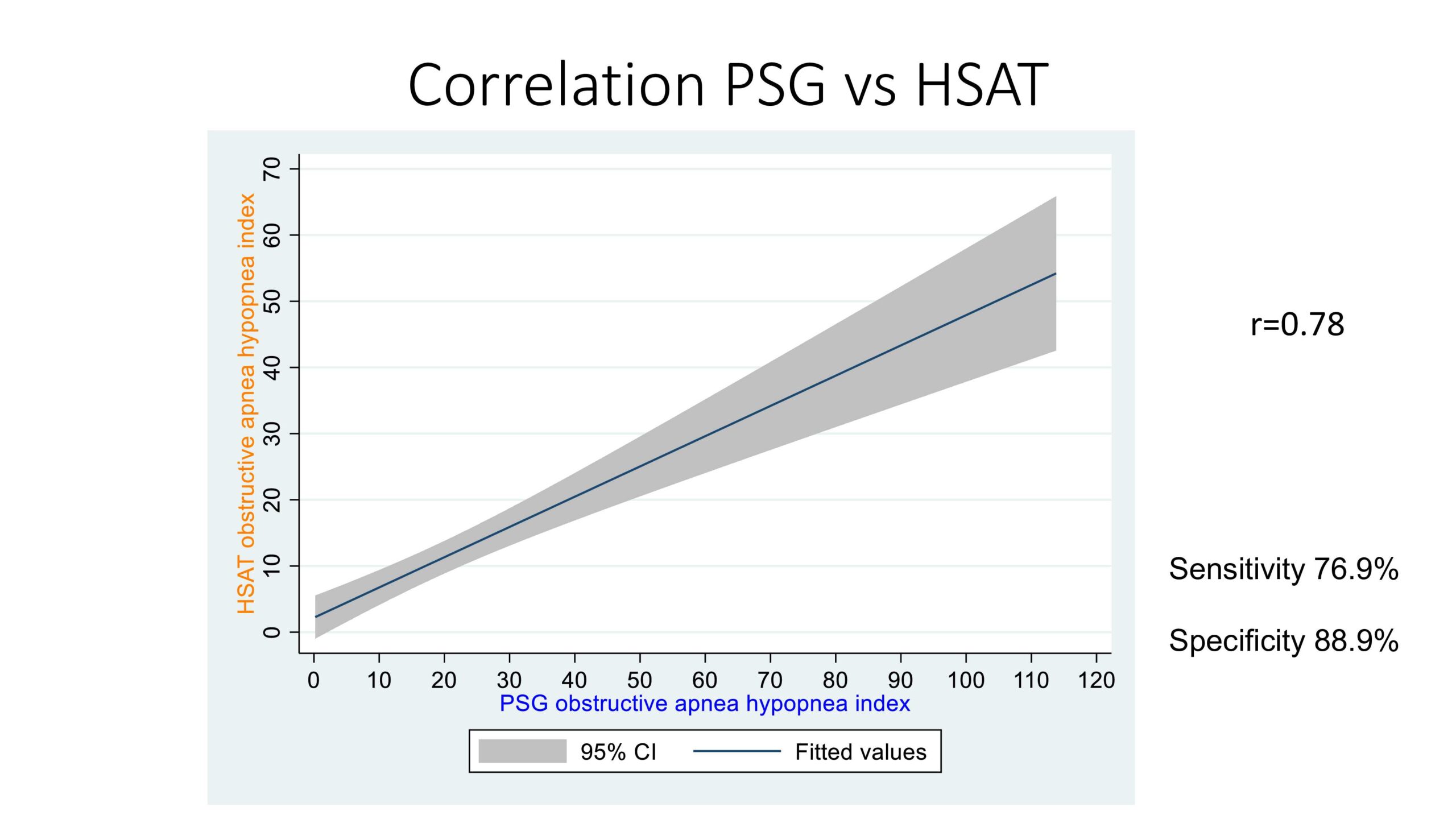
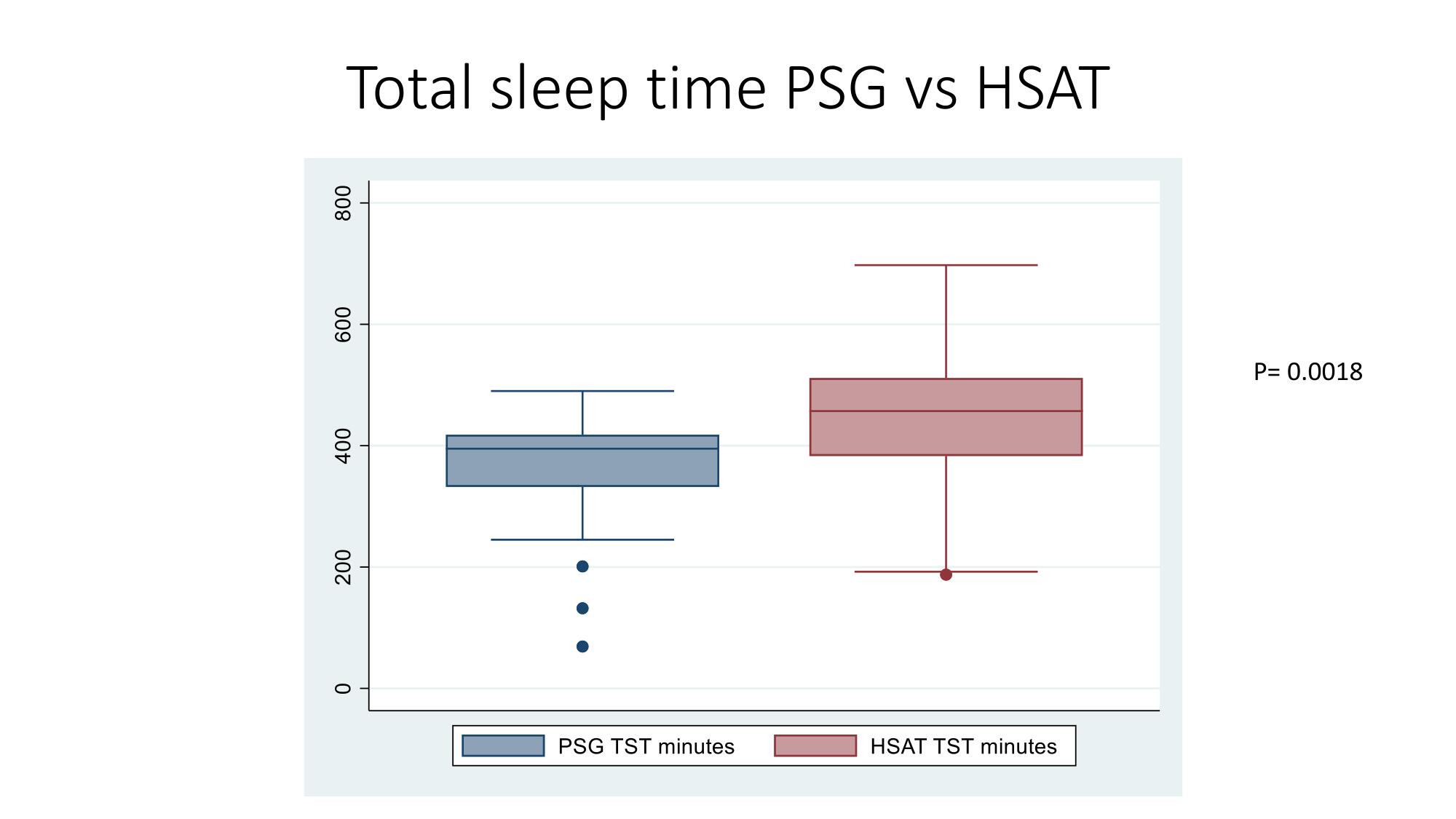
In terms of the accuracy, 78% of the home studies results correlated with the lab results on the obstructive apnea hypopnea index which is a very good score. Finally, the participants slept longer in the home study than during the lab study.
Dr. Tapia plans to continue his research and to address the following:
- What are the beliefs of families using CPAP or BiPAP over a most recent six-month period
- Strategies to increase PAP use
- Meet families where they are
- Bedtime routine
- Activities the child enjoys
- Role modeling
He concluded that families and patients with Down syndrome should redouble their efforts and engage a behavior specialist as his team is seeing a lot of success in patients with Down syndrome using the CPAP and making a huge difference in the patients’ energy level, focus and ability to participate more fully in all areas of life.
Treatment of OSA in Patients with Down Syndrome
Dr. Whelan, who is a sleep surgeon treating OSA in the general population as well as children and adults with Down syndrome, discussed treatment options for OSA. She discussed that continuous positive airway pressure (CPAP) is generally the first-line therapy in most adults with OSA. This works by delivering continuous pressure through the nose and/or mouth during the night to keep the upper airway open. While CPAP can be a challenge to acclimate to, CPAP may prove to ultimately be a very effective and well-tolerated treatment option for both children and adults with Down syndrome and OSA. If considering a trial of CPAP for your loved one, it is strongly advised to work with not only a sleep physician, but also a team that includes a behavioral sleep psychologist to help acclimate well to this new device.
Dr. Whelan discussed that different than in adults, the first-line of treatment for children with OSA in the United States is oftentimes Tonsillectomy & Adenoidectomy, removing the tonsils and adenoids by surgery.
While this surgery significantly improves or cures OSA in about 50% of children with Down syndrome, that still leaves about 50% of patients still having persistent OSA even after surgery. Because each patient has unique anatomy that leads to OSA, additional surgery is sometimes considered, including trimming or reshaping tissues in the nose, tongue, back of the throat, and/or around the voice box. Additional surgical options including weight-loss surgery (bariatric surgery) or skeletal surgery to expand the upper and/or lower jaws may also be considered.
Dr. Whelan agrees that the ongoing social stories sharing success around CPAP and BiPAP adherence is a wonderful success story for our community!
New Kid on the Block – Hypoglossal Nerve Stimulation
For non-obese patients that cannot tolerate CPAP or BPAP therapy, hypoglossal nerve stimulation (HNS) has become the newest surgical option to potentially treat OSA in patients with Down syndrome.
Dr. Whelan explained that HNS is like a pacemaker for sleep apnea and is a device inserted into a patient’s chest. There is another incision that sits under the chin and a wire is tunneled under the skin of the neck to connect the two parts of the device. It senses every breath the patient takes and sends electrical stimulations to push the tongue forward so that it does not fall back and block airflow in the back of the throat.
Hypoglossal nerve stimulation surgery is specifically for patients who have not had success with CPAP and who are not obese.
Adolescents with Down syndrome who have received HNS implants have overall done quite well. For the first 20 such patients there was significant improvement in OSA measures (pausing in breathing a median of 24 times per hour down to 3 times per hour) and improvements in speech, cognition, and school performance.
Based on this data, the Federal Drug Administration (FDA) recently approved HNS for 13 years or older patients with Down syndrome with moderate to severe OSA who have tried PAP and have not been successful with it. It is interesting to note that FDA approval in the general population is 18 years and older.
There are other important considerations regarding HNS implantation:
- The battery life generally lasts 10-12 years so patients require essentially one surgery each decade to replace the battery.
- MRI compatibility – while there is full body MRI compatibility with the current version of the device, this is a consideration for any patients that have medical conditions that will require frequent MR imaging.
- If patients gain weight, the device generally becomes less effective.
- Any time there is hardware, there are risks of infection or electronic failure of the device, which would require removing it.
Clinical trials to determine which patients respond best to this therapy are ongoing. Currently, there are five sites nationally enrolling adolescent patients with Down syndrome and OSA and looking at neurocognitive outcomes (focus, attention, executive function) before and after HNS implantation.
Dr. Whelan agrees that the current NIH INCLUDE funding is making a huge difference, allowing clinical researchers such as herself and Dr. Tapia to ask important questions about treatment such as:
- What are the patient centered outcomes and is there associated, appropriate neurobehavioral testing?
- What is the difference in daytime functioning?
- What is the difference in quality of life?
- Are there cardiometabolic outcomes?
- What are the family-centered outcome results?
- What are the risks/benefits for diagnosis and treatment?
Conclusions
Patients with Down syndrome are at high risk for sleep apnea. Obesity creates an even higher risk for OSA as well as other diseases so we should do our best to create healthy lifestyles and choices.
Detecting and treating OSA early and effectively can make a big difference in short-term health including behavior, attention and energy, as well as help limit serious long-term health issues such as heart disease, stroke risk and diabetes.
A sleep study is the only way to diagnose OSA and Dr. Tapia’s research is hoping to allow us to perform home sleep study tests rather than requiring an in-lab study, even in children with OSA.
To date, CPAP is the best way to treat OSA and great strides have been made in terms of behavioral interventions that allow children and adults with Down syndrome to tolerate a CPAP machine successfully.
For those who do not have a BMI in the obese range and have not had success with CPAP or BiPAP, there is a new treatment called Hypoglossal nerve stimulation that is very promising.
It is wonderful to envision a future where people with Down syndrome are allowed to and are willing to participate in long-term studies associated with OSA and sleep so that we can create better diagnosis, treatments, treatment supports and amazing health outcomes!
GLOSSARY
Adenotonsillectomy – An adenotonsillectomy is an operation to remove both the adenoids and tonsils; in other words a tonsillectomy and an adenoidectomy done at the same time
CPAP – Continuous positive airway pressure masks and head gear; the most common way to treat Obstructive Sleep Apnea (OSA)
BiPAP/BPAP – Bilevel positive airway pressure is a machine that helps you breathe; the most common way to treat Central Sleep Apnea (CSA), complex sleep apnea or chronic obstructive pulmonary disease (COPD) but can also be used to treat OSA
Glossoptosis – when the tongue is positioned further back in the mouth than normal; Abnormal posterior motion of tongue during sleep leading to OSA
Hypoglossal nerve stimulation – is a treatment for OSA using an implant to stimulate a nerve under the tongue to prevent the tongue from blocking the airway. As of 2023, the only hypoglossal nerve stimulator that is approved by the FDA is the Inspire device.
Hypoplasia – incomplete development or underdevelopment of an organ or tissue.
Hypothyroidism – also called underactive thyroid, is when the thyroid gland doesn’t make enough thyroid hormones to meet your body’s needs; The thyroid is a small, butterfly-shaped gland in the front of your neck
Hypotonia – decreased muscle tone
Midface hypoplasia – when the upper jaw, cheekbones and eye sockets have not grown as much as the rest of the face.
Polysomnography (PSG) – an overnight sleep study used to diagnose sleep disorders, recording
Obstructive Sleep Apnea Syndrome (OSAS) – excessive daytime sleepiness caused by OSA
brain waves, oxygen levels in your blood, your heart rate and movement
Recent Posts
- Bipartisan Congressional Members & Celebrities to Champion Down Syndrome Research in DC
- Global Down Syndrome Foundation Provides $16,000 in Employment Awards to Down Syndrome Organizations, Impacting over 5,000 people
- Global Down Syndrome Foundation Celebrates World Down Syndrome Day in Denver, NYC, Australia, Uganda & Italy
- Exclusive Interview with Down Syndrome Alabama Executive Director – Missy Haughery
- Join Headliners Phillip Phillips & Tucker Emry at GLOBAL’S AcceptAbility Gala in DC!

 Experience our inspirational and groundbreaking videos and photos. Our children and self-advocates are beautiful AND brilliant!
Experience our inspirational and groundbreaking videos and photos. Our children and self-advocates are beautiful AND brilliant! Make sure your local Representatives are on the Congressional Down Syndrome Task Force.
Make sure your local Representatives are on the Congressional Down Syndrome Task Force.