Decoding Dysphagia: Understanding Swallowing Challenges
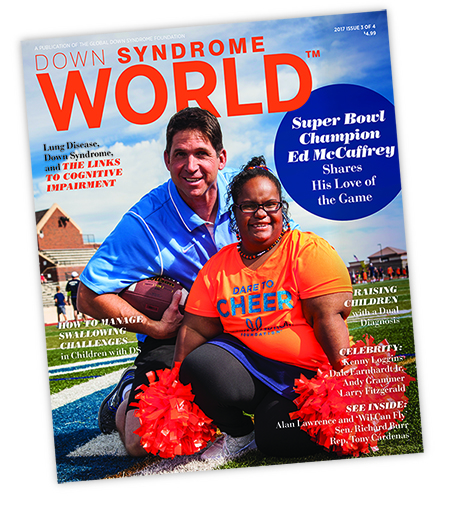
From Down Syndrome World Issue 3 of 4

Research shows that more than 50 percent of children with down syndrome who are referred for a swallow study are identified with swallowing problems, also known as dysphagia.
Since dysphagia can impact growth, nutrition, lung health, and participation in regular mealtime experiences, it is important for parents of children with down syndrome to know the potential signs of dysphagia and where to get help if a problem is suspected.
WHAT IS DYSPHAGIA?
Dysphagia can include difficulties in any of the three phases of swallowing:
- The oral phase, when the food/liquid is chewed and/or manipulated in the mouth to make it ready to swallow. Oral phase difficulties can include problems with extracting liquid from a breast, bottle, or cup, chewing, or controlling food/liquid in the mouth.
- The pharyngeal phase, when the food/liquid passes through the throat. Pharyngeal phase difficulties may include delay in starting the swallowing reflex, poor timing of closing off the airway before or during the swallow, and having residual material left in the throat after the swallow. These problems can lead to aspiration or entry of food/liquid into the airway.
- The esophageal phase, when the food/liquid passes from the throat through the esophagus to the stomach. Esophageal difficulties may include food/liquid moving slowly through the esophagus or getting stuck.
 This article was published in the award-winning Down Syndrome World™ magazine. Become a member to read all the articles and get future issues delivered to your door!
This article was published in the award-winning Down Syndrome World™ magazine. Become a member to read all the articles and get future issues delivered to your door!
Signs of dysphagia may include coughing, choking, having red/watering eyes, or sounding congested during or after feeding. Swallowing problems can also be silent, with no obvious signs or symptoms. In children who have frequent upper respiratory illnesses, pneumonia, or persistent oxygen requirement, doctors may suggest having swallowing evaluated, even if there are no clear signs of a problem.
HOW IS DYSPHAGIA DIAGNOSED?
If the child appears to be having problems only in the oral phase of the swallow, a feeding evaluation, during which a child’s feeding skills are observed by a specialist or team of specialists, may be recommended.
If compromised airway protection is suspected, the child’s doctor may order an imaging study. The two most common imaging studies used to diagnose swallowing problems are the videofluoroscopic swallow study (VFSS) and the fiberoptic endoscopic evaluation of swallowing (FEES). The VFSS is done in the radiology department and looks like a “moving X-ray” of the head and neck.
The FEES is typically conducted in the office of an ear, nose, and throat doctor, also known as an otolaryngologist. During the FEES, a small, flexible tube called an endoscope is inserted into the child’s nasal passages. The endoscope is attached to a bright light and a camera, which allow the team to view the inside of the nose and throat.
During the VFSS and the FEES, the swallow team, including a speech-language and/or occupational therapist and a physician (either a radiologist for VFSS or an otolar yngologist for FEES) observes aspects of the child’s swallowing function, such as his or her ability to clear the throat between swallows and protect the airway during swallowing. If a problem is detected, the swallow team may try different strategies to improve swallowing, such as offering a slower-flowing bottle nipple or changing the child’s position.
If difficulties of the esophageal phase of swallowing are suspected, an imaging study completed in radiology called an upper GI or esophagram may be ordered.
HOW CAN I HELP MY CHILD WITH A SWALLOWING PROBLEM?
The most important way that parents and medical providers can help children with dysphagia is to take steps to protect their children’s lungs, as ongoing aspiration can negatively impact pulmonary health. An evaluation with a pulmonologist for further assessment of lung health may be beneficial. Children with severe or persistent dysphagia may be referred to other medical specialists, such as an otolaryngologist or neurologist, for further evaluation as to the cause of the swallowing problem.
Maintaining adequate nutrition and hydration is another critical component of caring for children with swallowing problems. A dietician and/or gastroenterologist may be involved in the child’s care. After the swallow study, the evaluating team will provide recommendations about types of food and liquid that the child is able to swallow most safely. Modifying the child’s diet by minimizing exposure to foods that are more likely to be aspirated and offering foods that can be swallowed safely is an important step that can be taken to give the child the consistent experience of swallowing food and liquid with minimal aspiration.
For children who have severe dysphagia and are unable to swallow any food or liquid without aspirating, providing ongoing positive stimulation to the mouth through play, textured toys, and controlled experiences with small amounts of food and liquid (if approved by the medical team) can help the child maintain and develop skills for using his or her mouth.
Feeding and other developmental therapists can provide helpful services to children with swallowing disorders by teaching skills that support safe and functional feeding and swallowing. Those skills may include teaching the family appropriate positioning and pacing of the mealtime, working on underlying control and strength at the core of the body, and helping children control food or liquid more effectively in the mouth. It is important that therapy for feeding and swallowing issues is individualized for each child and addresses the areas of difficulty identified during the child’s feeding or swallowing evaluation.
PARENT TIPS FOR SWALLOW STUDIES
BEFORE THE STUDY:
- Find out what to expect during the swallow study. For example, will it be a videofluoroscopic swallow study or a fiberoptic endoscopic evaluation of swallowing? Will you be able to feed your child? What will
your child be eating and drinking? - Contact the swallow team ahead of time to make a plan that will work best for your child if you are concerned about whether your child will participate. Many hospitals have child life specialists who can help children be more comfortable during medical tests.
- Be aware that the swallowing team may make recommendations to change your child’s diet to help them swallow more safely.
DURING THE STUDY:
- Help the swallow team to support your child. Bring preferred cups, plates, utensils, foods, and drinks from home. Tell the team if your child has special routines that help him or her eat or drink.
- Make sure you understand the results and recommendations before you leave the appointment. Ask for clarification if you are unsure how to follow the recommendations at home.
AFTER THE STUDY:
- Discuss the results with your child’s doctor and/or medical team.
- Find out who to contact if your swallowing recommendations are not working or if you have follow-up questions.
—-
If your child’s pediatrician recommends a swallow study, visit a medical care center that specializes in treating patients with Down syndrome. Find one at bit.ly/global-medical-care.
About the Authors
Arwen Jackson, M.A., CCC-SLP, and Jennifer Maybee, OTR, M.A., CCC-SLP, are both speech-language pathologists and feeding and sw allowing specialists at the Anna and John J. Sie Center for Down Syndrome at Children’s Hospital Colorado. They work with parents and individuals with Down syndrome to manage dysphagia through the Sie Center’s weekly Feeding Clinic.
References
- Frazier, J. B., and Friedman, B. (1996). Swallow function in children with Down syndrome: a retrospective study. Developmental Medicine & Child Neurology, 38, 695–703.
- Jackson, A., Maybee, J., Moran, M. K., Wolter-Warmerdam, K., and Hickey, F. (2016). Clinical characteristics of dysphagia in children with Down syndrome. Dysphagia, 1–9.
- O’Neill, A. C., and Richter, G. T. (2013). Pharyngeal dysphagia in children with Down syndrome. Otolaryngology – Head and Neck Surgery, 149(1), 146–150.
Like this article? Join Global Down Syndrome Foundation’s Membership program today to receive 4 issues of the quarterly award-winning publication, plus access to 4 seasonal educational Webinar Series, and eligibility to apply for Global’s Employment and Educational Grants.
Register today at downsyndromeworld.org!

 Experience our inspirational and groundbreaking videos and photos. Our children and self-advocates are beautiful AND brilliant!
Experience our inspirational and groundbreaking videos and photos. Our children and self-advocates are beautiful AND brilliant! Make sure your local Representatives are on the Congressional Down Syndrome Task Force.
Make sure your local Representatives are on the Congressional Down Syndrome Task Force.